Thalassaemia International Federation applauds FDA approval of SCD gene therapies
The US Food and Drug Administration (FDA) simultaneously approved two innovative gene therapies for individuals with sickle cell anaemia last week, offering substantial hope for a radical treatment of this severe haematological disorder.
The two therapies are Casgevy (exa-cel) by Vertex Pharmaceuticals and CRISPR Therapeutics – the world’s first drug to utilise the revolutionary CRISPR gene-editing system which earned its creators the 2020 Nobel Prize in Chemistry –, and bluebird bio’s Lyfgenia (lovo-cel), for patients 12 years and above with a history of vaso-occlusive crises (VOCs), the most severe and painful symptom of sickle cell anaemia.
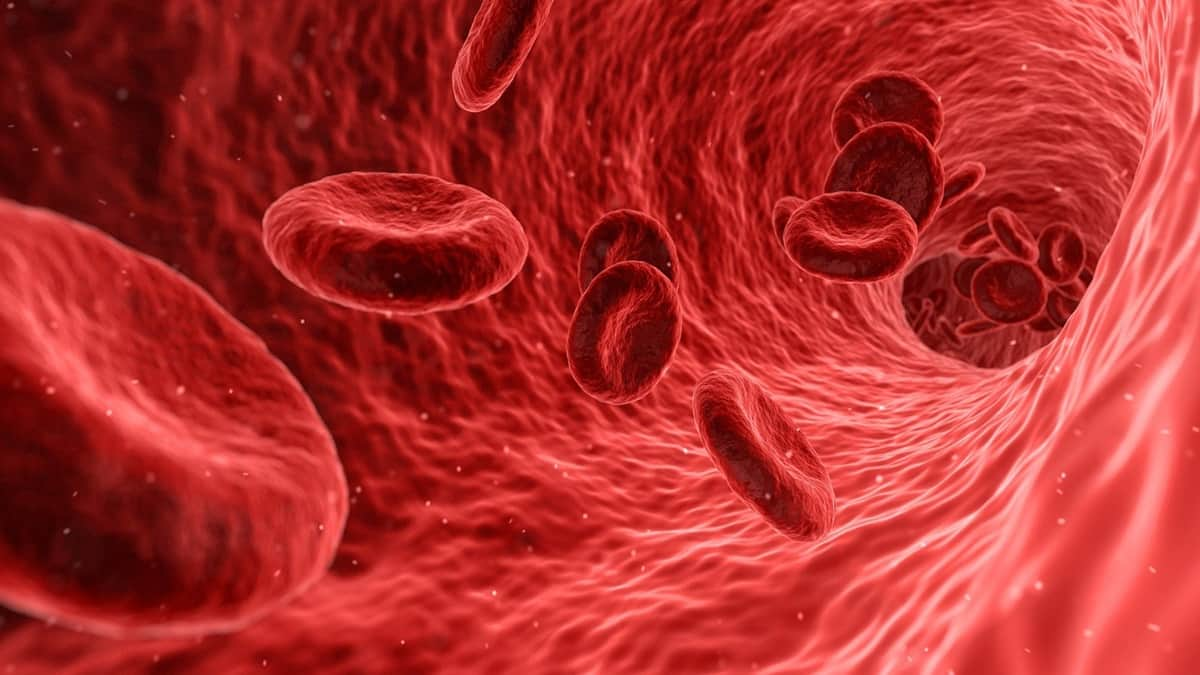
Sickle cell disease is an inherited haematological disorder causing abnormal red blood cell growth. The cells become stiff and sickle-shaped, obstructing normal blood flow, and reducing oxygen transport to tissues and organs. It affects at least 100,000 people in the United States and millions of patients worldwide, with a higher prevalence among people of African and Mediterranean descent.
Casgevy’s approval in the US follows its approval in the UK for both sickle cell anaemia and beta-thalassaemia indications, with Bahrain following suit last week. Casgevy is under review in the US for transfusion-dependent beta-thalassaemia, with a decision anticipated by March 2024. The European Medicines Agency will also decide whether to approve the therapy within the next year.
“We are truly witnessing history, as these approvals mark not only a major advancement for those living with sickle cell disease but also the beginning of a new era in treating numerous debilitating genetic conditions,” states Dr. Androulla Eleftheriou, Executive Director of the Thalassaemia International Federation (TIF). However, she acknowledges that “these groundbreaking treatments come with challenges. The logistical complexity of gene therapies, their high costs, and bureaucratic hurdles within many national healthcare systems may delay their integration and reimbursement, ultimately affecting availability to those in need.”
Inclusive health policies, proactive infrastructure development, mature regulatory environments, and the establishment of flexible financing models and reimbursement strategies are critical components in expanding access to these life-saving treatments, TIF stated.
“The Thalassaemia International Federation (TIF) is committed to supporting, educating, and advocating for the rights and needs of individuals with thalassaemia and other hemoglobinopathies worldwide. TIF firmly believes that patients must be given the choice to access all available, approved, and safe treatment options—regardless of cost—to uphold their right to the best possible quality of life. Governments ought to prioritize addressing the availability and accessibility of these innovative treatments for eligible patients,” the organisation said in a statement.